Medical documentation is an essential part of clinical practice, serving not only as a record of patient care but also as a communication tool among healthcare providers. One of the most widely used methods for documenting patient encounters is the SOAP note, an acronym for Subjective, Objective, Assessment, and Plan. This format provides a structured way to capture patient data, ensuring consistency, clarity, and completeness. With the advent of Electronic Health Record (EHR) software, the integration of SOAP notes into digital platforms has further revolutionised medical documentation, enhancing both the quality of care and the efficiency of clinical operations.
The Components of a SOAP Note
SOAP notes offer a systematic approach to clinical documentation, breaking down the patient encounter into four distinct sections:
Subjective (S): This section records the patient’s history and symptoms as described by the patient. It includes the chief complaint, history of present illness, past medical history, family history, social history, and a review of systems. The subjective information is essential for understanding the patient’s perspective and forms the foundation for the subsequent sections of the SOAP note.
Objective (O): The objective section contains measurable, observable data collected during the clinical encounter. This includes physical examination findings, vital signs, laboratory results, imaging studies, and other diagnostic information. This section provides the clinician with concrete evidence to support or refute the patient’s subjective complaints.
Assessment (A): The assessment section is where the clinician synthesises the subjective and objective information to arrive at a diagnosis or a differential diagnosis. This section may also include a discussion of the patient’s progress, the effectiveness of previous treatments, and any changes in the clinical picture.
Plan (P): The plan outlines the next steps in the patient’s care, including diagnostic tests, treatments, referrals, and follow-up appointments. This section also serves as a communication tool, ensuring that all members of the healthcare team are aware of the patient’s care plan and their role in its execution.
Importance of SOAP Notes
SOAP notes are vital in several ways:
Consistency and Structure: The structured format of SOAP notes ensures that all aspects of the patient encounter are documented systematically. This consistency is crucial for maintaining comprehensive and accurate records, which are essential for continuity of care, particularly when multiple healthcare providers are involved.
Communication: SOAP notes facilitate clear communication among healthcare providers. The structured format makes it easy for clinicians to quickly review a patient’s history, current status, and treatment plan, ensuring that all members of the care team are on the same page.
Legal Documentation: SOAP notes serve as legal documents that can be used in medical audits, insurance claims, and legal cases. Accurate and detailed documentation can protect healthcare providers from legal disputes and malpractice claims.
Clinical Decision-Making: By systematically capturing patient data, SOAP notes help clinicians make informed decisions about diagnosis and treatment. The process of synthesising subjective and objective information into an assessment and plan encourages critical thinking and clinical reasoning.
Integration of SOAP Notes into EHR Software
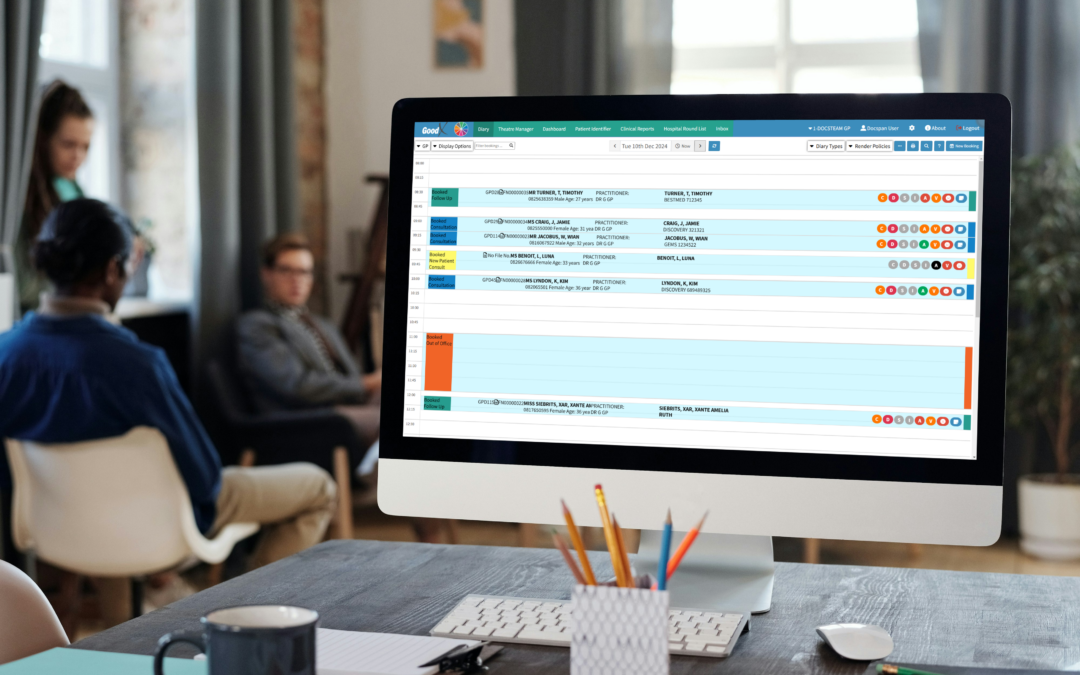
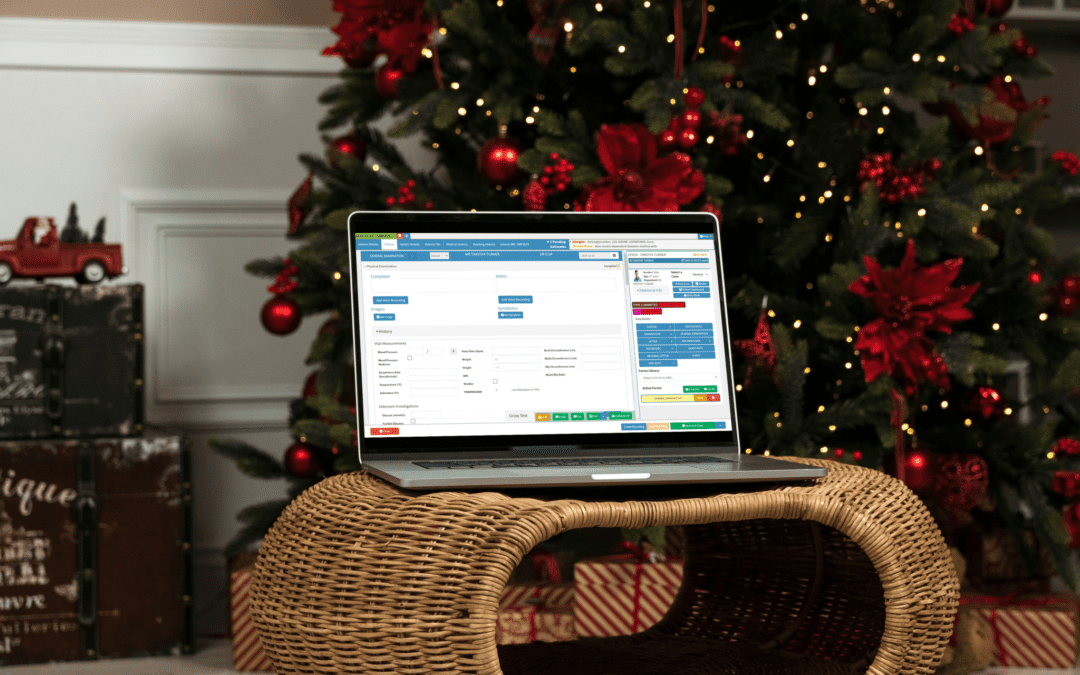
With the digital transformation of healthcare, the integration of SOAP notes into EHR software has become increasingly common. EHRs are digital versions of patients’ paper charts and are designed to streamline and improve the quality of care. Integrating SOAP notes into EHR systems offers numerous benefits:
Improved Accessibility and Efficiency: EHRs allow for the instant retrieval of patient information, making it easier for clinicians to access and review SOAP notes. This reduces the time spent on documentation and frees up more time for patient care. Additionally, EHRs can be accessed remotely, allowing clinicians to review and update patient information from any location.
Enhanced Accuracy and Completeness: EHR software often includes templates and prompts that guide clinicians through the documentation process, helping to ensure that all relevant information is captured. This reduces the risk of omissions or errors in documentation, improving the accuracy and completeness of SOAP notes.
Interoperability and Collaboration: EHRs facilitate the sharing of patient information across different healthcare providers and settings. This interoperability enhances collaboration among care teams, allowing for more coordinated and integrated care. SOAP notes documented in an EHR can be easily shared with specialists, hospitals, and other healthcare providers, ensuring that everyone involved in the patient’s care has access to the same information.
Data Analytics and Clinical Decision Support: EHRs can aggregate and analyse data from multiple patient encounters, providing clinicians with valuable insights and clinical decision support. For example, EHRs can flag potential drug interactions, suggest evidence-based treatment options, or alert clinicians to abnormal lab results. By integrating SOAP notes into these systems, clinicians can leverage these tools to enhance clinical decision-making and improve patient outcomes.
Compliance and Reporting: EHR software can help healthcare providers meet regulatory requirements and quality standards by ensuring that SOAP notes are complete and compliant with industry guidelines. EHRs can also generate reports and dashboards that track key performance indicators, helping organisations monitor and improve the quality of care.
Challenges and Considerations
While the integration of SOAP notes into EHR systems offers numerous benefits, it also presents certain challenges. One common concern is the potential for “copy-paste” errors, where clinicians may inadvertently duplicate information from previous notes without updating it for the current encounter. This can lead to inaccuracies and compromise the quality of documentation. Additionally, some clinicians may find the use of EHR templates restrictive, limiting their ability to document patient encounters in detail.
To address these challenges, healthcare organisations need to provide training and support to clinicians on the effective use of EHR systems. This includes educating clinicians on best practices for documenting SOAP notes, such as using templates as a guide rather than a rigid framework and ensuring that notes are updated and personalised for each patient encounter.
SOAP notes play a critical role in medical documentation, offering a structured and systematic approach to capturing patient information. Integrating SOAP notes into EHR software can enhance the quality of care, improve efficiency, and facilitate collaboration among healthcare providers. However, it is important for healthcare organisations to address the challenges associated with digital documentation and to ensure that clinicians are equipped with the tools and training needed to utilise EHR systems effectively. By doing so, they can harness the full potential of SOAP notes and EHRs to improve patient care and outcomes.
References
- Weed, L. L. (1968). Medical Records, Medical Education, and Patient Care. The Problem-Oriented Record as a Basic Tool. Archives of Internal Medicine, 122(2), 255–264.
- Heathfield, H., Pitty, D., & Hanka, R. (1998). Evaluating information technology in health care: barriers and challenges. BMJ, 316(7149), 1959–1961.
- Bowman, S. (2013). Impact of electronic health record systems on information integrity: quality and safety implications. Perspectives in Health Information Management, 10(Winter), 1c.